Colic is a major frustration for many new parents, but it’s not a diagnosis in itself. Instead it is a collection of symptoms- a syndrome. The main symptom is more frequent or longer periods of crying than normal, which are often worse in the evening than the rest of the day.
Symptoms of Colic
The diagnostic criteria of colic has been updated to cover babies who:
cry for more than three hours a day
for at least three hours a week
over a period of at least one week
This criteria does not apply if there is another explanation for the crying.
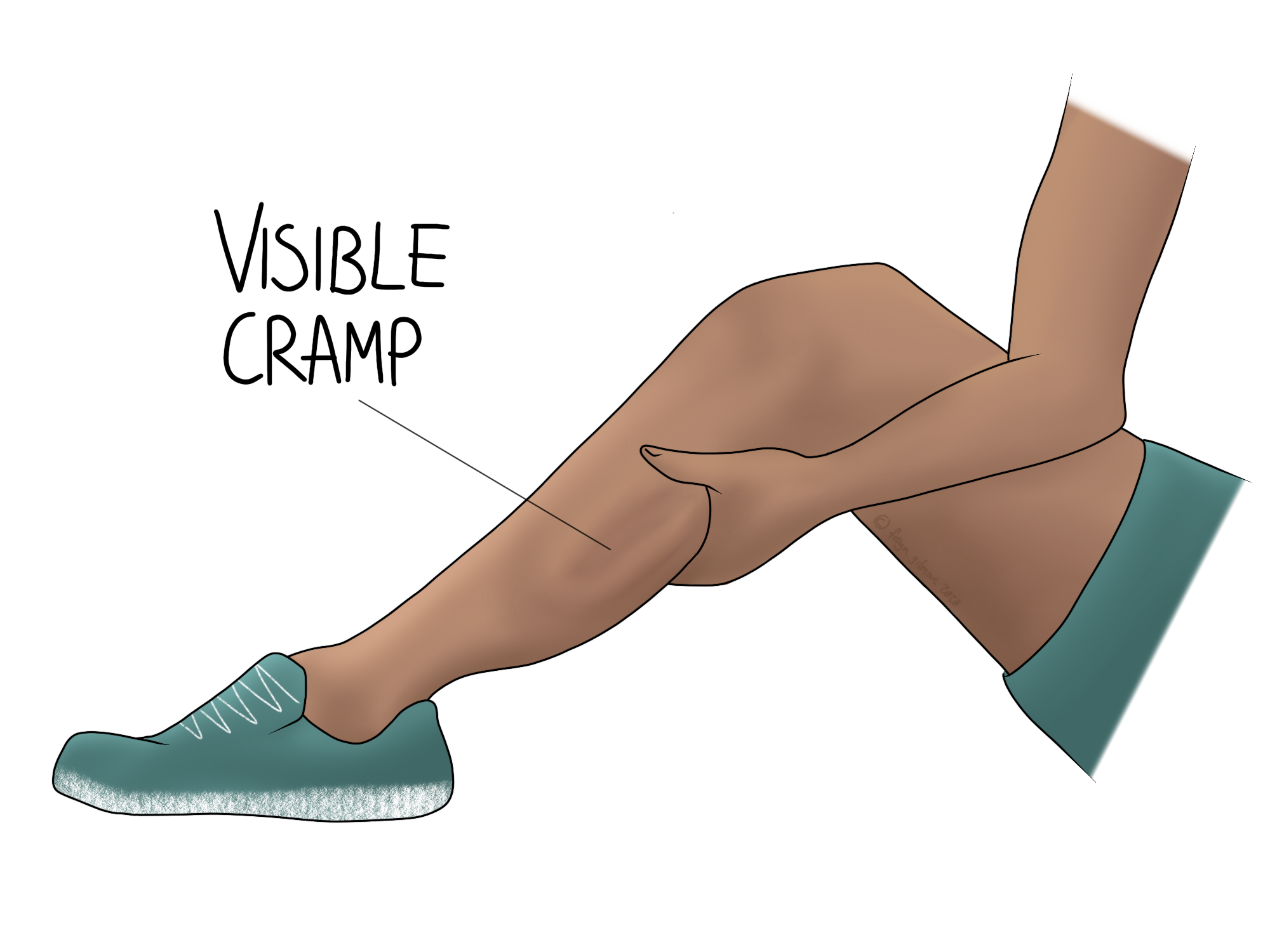
Beyond the extended periods of crying, symptoms can also include signs of abdominal discomfort, going red in the face, and clenching their fists. Although its impact on the family can be huge, colic only affects babies for a small period of time. By the age of 3 or 4 months, it should self resolve.
Cause for Investigation
As little babies are unable to effectively communicate, we have to consider that their discomfort is something more serious. Colic symptoms lasting beyond 4 months of age should be investigated by your GP.
This is also a situation where you should trust your gut. If you feel that something is not quite right, don’t feel that you would be wasting anyone’s time to have your baby checked out.
Possible Explanations
As colic is not a diagnosis, it does not come with a blanket explanation for why it occurs.
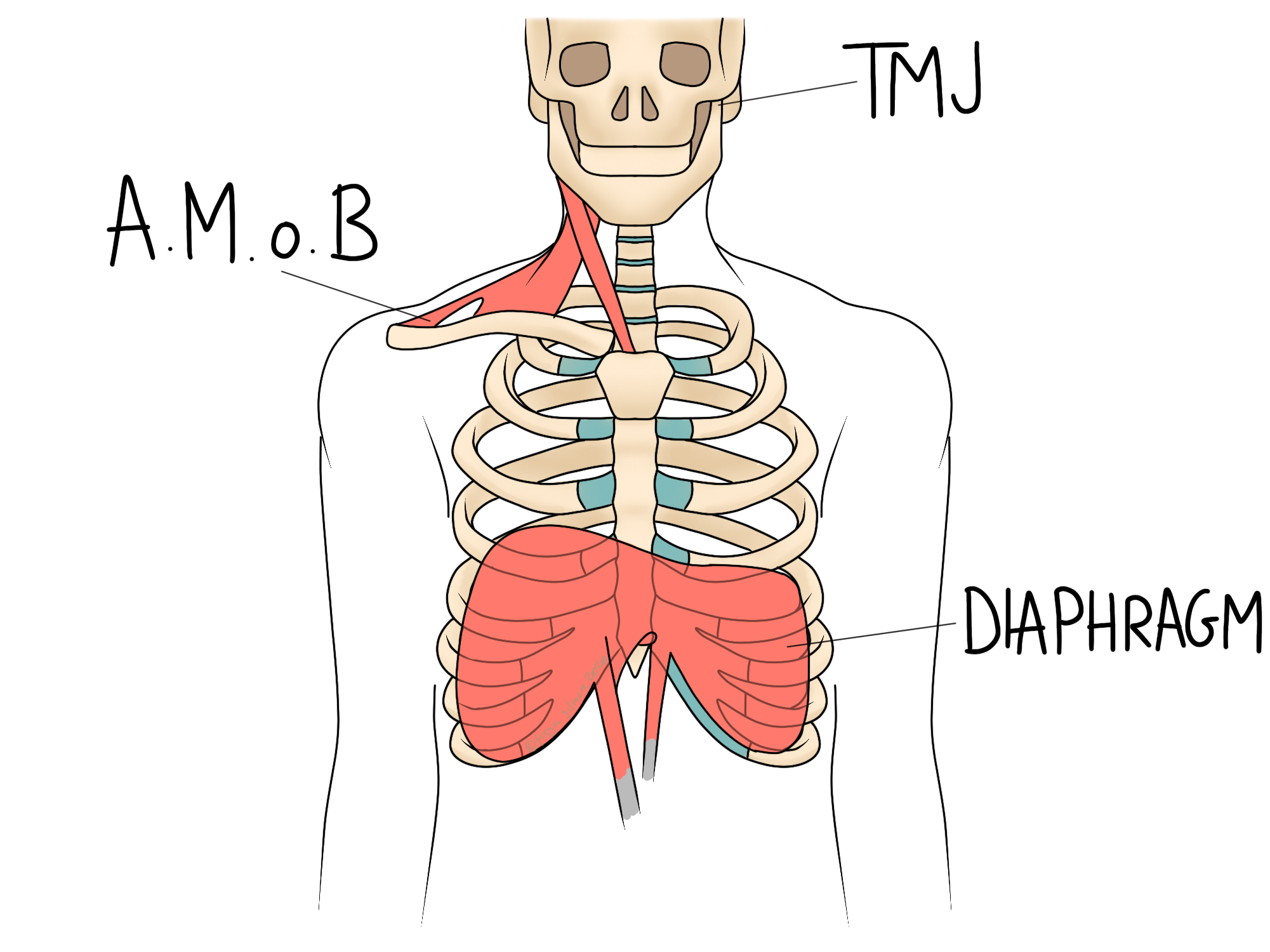
Often there seem to be digestive links, and indeed some of the recognised symptoms of colic are also recognised symptoms of reflux. An arched back, and knees brought up to the chest are good examples of this crossover. Common advice to ensure to wind your baby after feeds could also help to address reflux if that does form part of your baby’s picture of colic.
You can read more about infant reflux here.
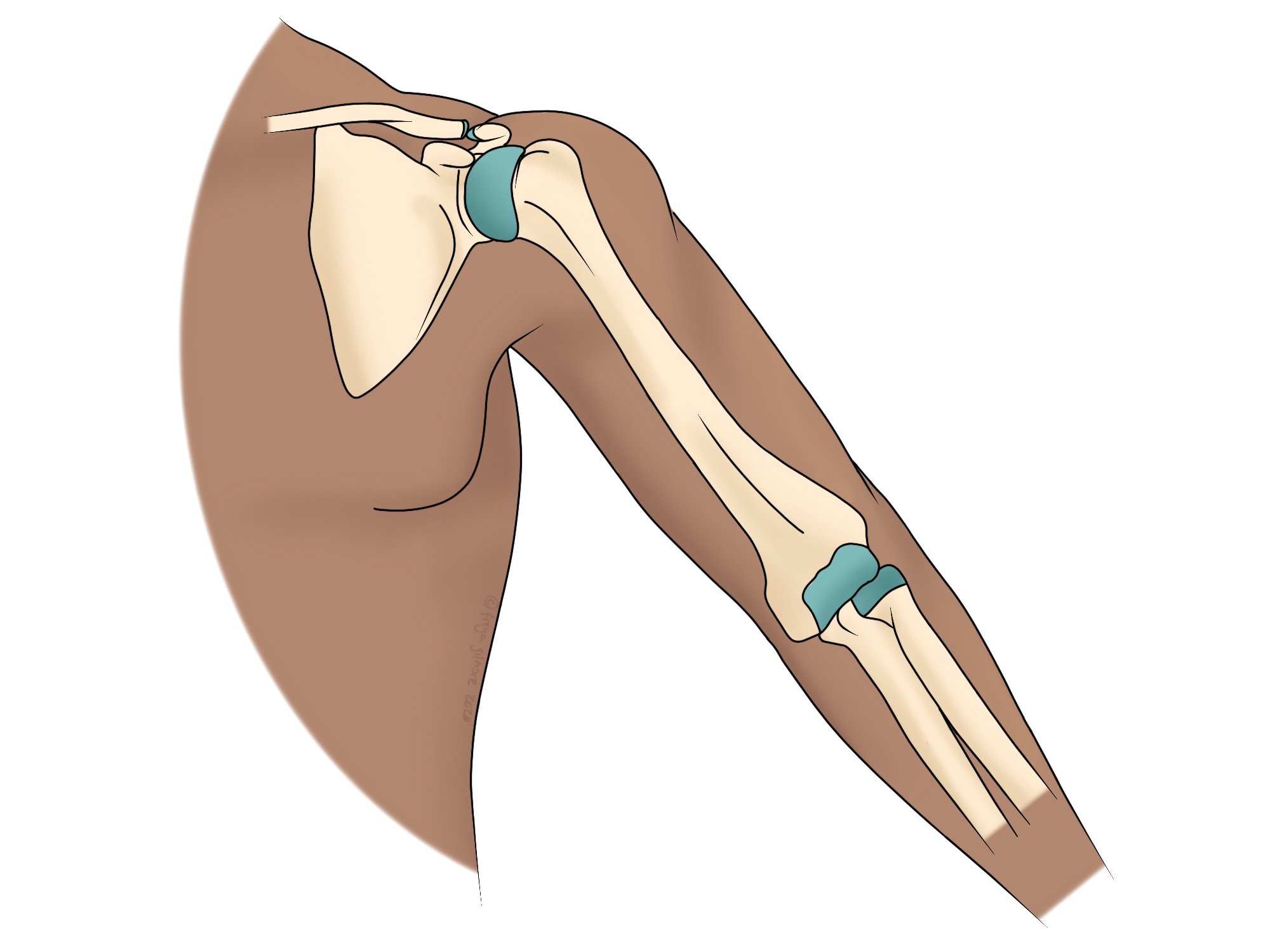
In the first four months of life, a baby goes through huge changes. Physically, their bones are growing at an unprecedented rate, and we know in older children that growing pains can be very sore. It is possible that this kind of pain is part of the problem.
Osteopathy and Colic
Evidence for any form of treatment for colic is severely lacking, but steps are being made to research treatment options. Some parents find that gentle osteopathic treatment helps their babies to be more settled. Light-touch work to the joints of the skull, or massage-type techniques for the abdomen may help to settle your baby. A paediatric trained osteopath can also help to stretch out any tight muscles that may be playing a role, and show you how to keep the progress going at home.
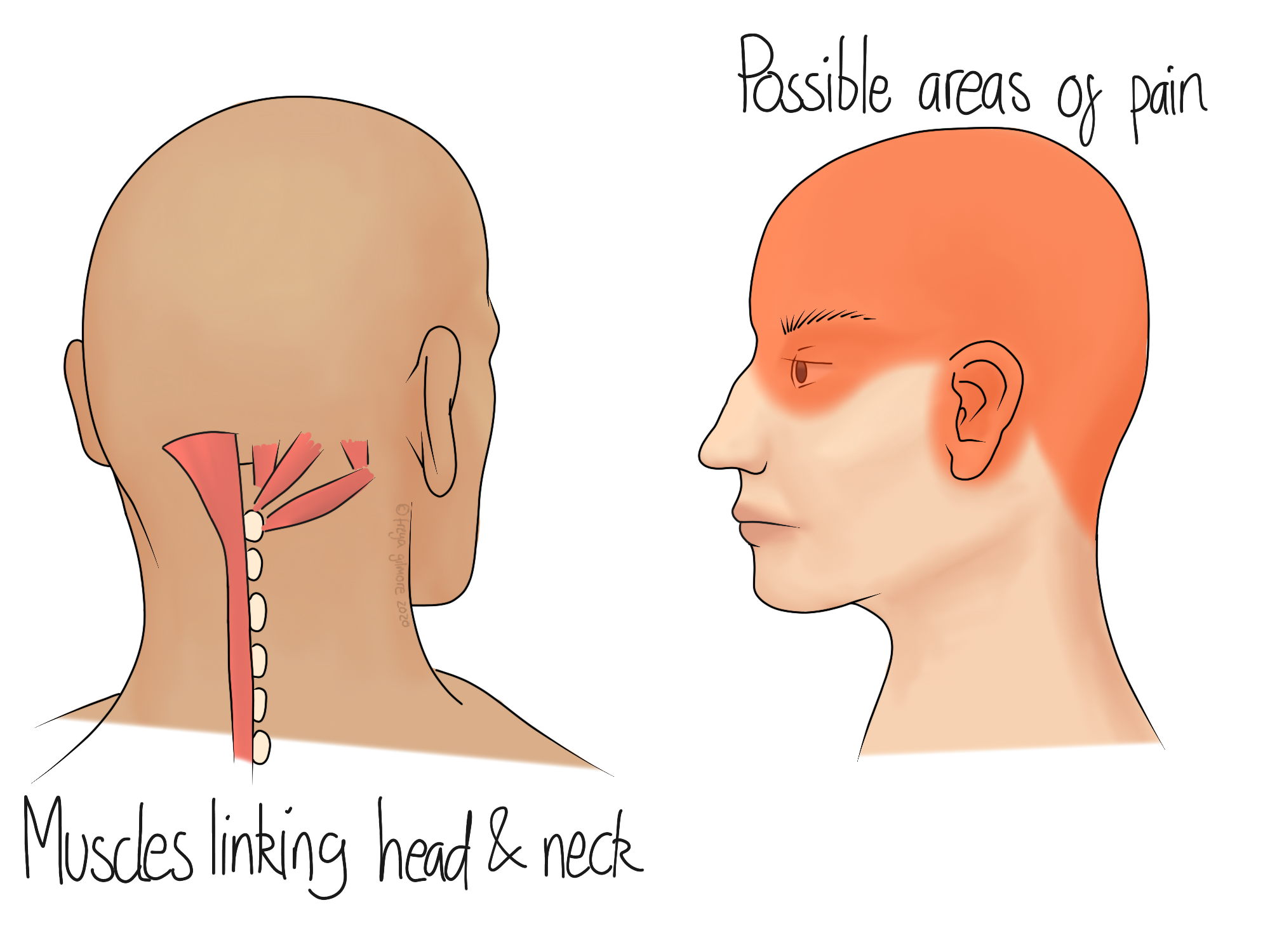
As a parent, having a baby with colic can be very stressful. This alone can cause tension in the shoulders, associated with upper back pain or headaches. The advice to hold or rock your baby during an episode might further exacerbate this, but you will likely find yourself at the bottom of your list of priorities. Your osteopath can help your aches and pains as you navigate your baby’s colicky season.